
Best practices aren't accidental. Like Aristotle's virtues, they are refined and reinforced by habit.
"For colonoscopy, there are things that you may not be doing in the endoscopy unit, but should," said Charles J. Kahi, MD, MSc, professor of medicine at Indiana University School of Medicine, and chief of the GI section at the Richard L. Roudebush VA Medical Center, both in Indianapolis. In an invited lecture at the 2017 Digestive Disease Week, Dr. Kahi discussed components of colonoscopy that can help prevent interval colorectal cancer and improve the quality of the examination.
"In 2017, a split-dose bowel prep should be the standard of care," Dr. Kahi said. Many high-quality studies have documented that adenoma detection improves with the systemwide adoption of split preps. Split-dose bowel prep is now strongly recommended for elective colonoscopy by the U.S. Multi-Society Task Force.
In a meta-analysis of 32 trials of several different bowel preparation products, patients receiving a split-dose prep were 2.5 times more likely to have excellent or good bowel cleansing, and almost twice as willing to repeat the same prep for a subsequent colonoscopy, as those who took a day-before prep (Gastroenterology 2015;149:79-88).

Charles J. Kahi, MD, MSc
Studies have also shown improvements in adenoma detection rates (ADRs) and the identification of advanced adenomas. "This can have a significant impact on preventing CRC," Dr. Kahi said.
Dr. Kahi also advised clinicians to attempt salvage measures for patients who have brown effluent despite compliance with prep instructions; to grade the prep after lavage, not before efforts to clean; and if the prep is still judged inadequate after a complete colonoscopy, to repeat the colonoscopy within one year using a more intensive prep regimen.
"Right colon retroflexion has gained attention recently as a modality to increase the yield for adenomas," Dr. Kahi said.
A meta-analysis of eight randomized controlled trials aimed to determine the effect of right colon retroflexion on improving ADRs compared with conventional colonoscopy without retroflexion (J Clin Gastroenterol 2016 Sep 28. [Epub ahead of print]).
Colonoscopy with right-sided retroflexion significantly increased adenoma detection in the right colon; the adenoma miss rate—defined as the number of additional adenomas found in the right colon in retroflexion divided by the total number of adenomas found in both forward and retroflexed views—was 17%. Adverse events were limited to one perforation in one patient (0.03%). The authors concluded that reexamination of the right colon in retroflexed view should be strongly considered for quality improvement in colon cancer prevention.
"The obvious next question is whether right colon retroflexion is a 'right colon reexamination in disguise,'" Dr. Kahi said.
In other words, can the increased yield be attributed simply to examining the colon a second time?

A multicenter trial involving 850 patients addressed this question, randomly assigning patients to a second right colon forward-view exam or right colon retroflexed exam (Am J Gastroenterol 2015;110:415-422). The ADR and detection of adenomas per patient were found to be similar between the two groups.
At least one additional adenoma was detected in 10.5% of patients with forward-view colonoscopy and in 7.5% with retroflexion (P=0.13). The strongest predictors for finding adenomas on the second examination were presence of adenomas on the first examination (odds ratio [OR], 2.8) and low endoscopist confidence about the quality of the first examination (OR, 4.8).
Dr. Kahi advised that in higher-risk situations when adenomas could be missed, clinicians should consider reexamining the right colon. These factors include older age, male sex, bleeding indication for colonoscopy, presence of anemia and neoplasia identified on first pass. "If you have found several polyps, there's a good chance there are several others you haven't seen," he said.
"My preference is to always examine the right colon twice, and to try doing it in retroflexion," he said. "It can be a valuable technique for certain polypectomies when polyps are in a challenging location."
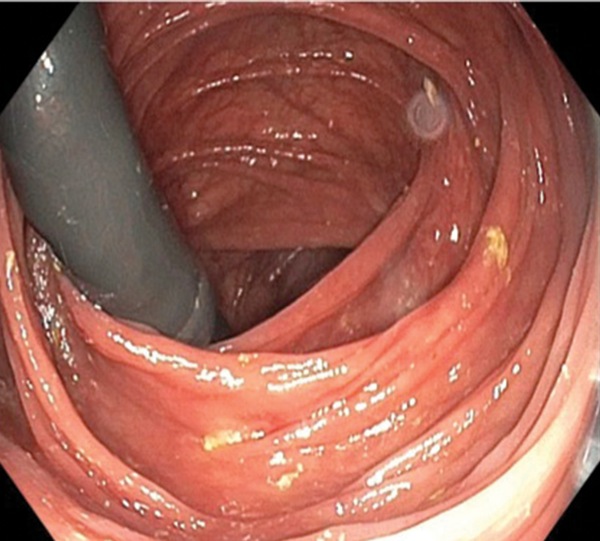
Figure. View of the right colon in retroflexion.
"Carbon dioxide has been gaining traction," Dr. Kahi said. "It's hard not to be a fan."
The gastrointestinal tract absorbs CO2 160 times faster than it does nitrogen, and CO2 is eliminated rapidly by the lungs. Compared with air insufflation, CO2 is associated with less discomfort in unsedated colonoscopy, lower sedative doses in on-demand sedation colonoscopy, less pain after procedures with sedation, less abdominal distention and girth, and improved patient satisfaction.
Some of these advantages were shown in a meta-analysis of 21 randomized trials involving 3,607 patients (Colorectal Dis 2015;17:111-123). The only factor that did not improve relative to air insufflation was the rate of cecal intubation, although time to reach the cecum was shorter with CO2.
The greatest barrier to the use of CO2 is probably cost, Dr. Kahi noted. Capital expenditures run $4,500 to $8,000 for a CO2 insufflator system, with additional outlays for tubing, bottle caps and cylinders. However, an analysis by the American Society for Gastrointestinal Endoscopy determined that once the system is in place, the use of CO2 adds only $3 to the cost of each colonoscopy (Gastrointest Endosc 2016;83:857-865). "This seems a small expense for the advantages you get," he said.
Water-assisted procedures reduce the need for sedation and improve completion rates in unsedated patients; help clinicians complete difficult exams; and can increase adenoma yield over air insufflation, as shown in a recent study of water exchange (Endoscopy 2017;49:456-467).
Although Dr. Kahi said he does not recommend the routine use of water-based techniques, he acknowledged that the approach is gaining acceptance and requires further exploration in clinical trials.
For the removal of small and diminutive polyps, cold snare techniques outperform cold forceps in terms of the completeness of polypectomy, according to Dr. Kahi. A meta-analysis found that cold snare reduced incomplete histologic eradication by 69% (Gastrointest Endosc 2016;83:508-515).
Dr. Kahi pointed out that cold snare eliminates electrocautery-related complications and avoids piecemeal forceps resection. He said he uses cold snare on most polyps less than 10 mm, reserving the use of cold forceps for flat polyps of 1 to 2 mm, in situations when the scope cannot be rotated to view polyps in the left endoscopic field, and when polyps can be "engulfed in one bite, with partly open jaws."
The overarching message, Dr. Kahi stressed, is that clinicians must strive to meet quality metrics during all aspects of colonoscopy. "Quality is not just about one metric," he said. "It's the linchpin of what we do and the cornerstone of cancer prevention. The most important thing we should be doing is assessing and improving colonoscopy quality."